More Information
Submitted: 24 January 2020 | Approved: 14 April 2020 | Published: 15 April 2020
How to cite this article: Sidhu HS, Sandeep S. Primary anal malignant melanoma: A case report. J Radiol Oncol. 2020; 4: 001-004.
DOI: 10.29328/journal.jro.1001031
Copyright License: © 2020 Sidhu HS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Anal canal; Malignant melanoma; Magnetic Resonance Imaging (MRI)
Primary anal malignant melanoma: A case report
Harsumeet S Sidhu* and Sonia Sandeep
Department of Radiodiagnosis, Dr. RML Hospital, New Delhi-110001, India
*Address for Correspondence: Harsumeet S Sidhu, Department of Radiodiagnosis, Dr. RML Hospital, New Delhi-110001, India, Email: [email protected]
Anal melanoma is a rare and highly aggressive mucosal melanocytic malignancy. It is the third most common after melanomas of the skin and retina. The peak incidence in seen in the sixth and seventh decades. The clinical symptoms are pain, anal mass, bleeding per rectum, tenesmus or change in the bowel habits. It affects anal canal, rectum or both with a tendency to spread along submucosal planes. It is mostly beyond complete resection at the time of diagnosis and majority of patients die of metastasis. MR imaging significantly increases the diagnosis of anal melanoma in its early stages.
We report a case of 60 year old male who presented to the out-patient department with a four months history of perianal pain and bleeding per rectum. Bleeding was associated with defecation and the blood was bright red in colour with few intermittent episodes of dark clotted blood. Digital examination of rectum revealed firm thickening of anal canal wall.
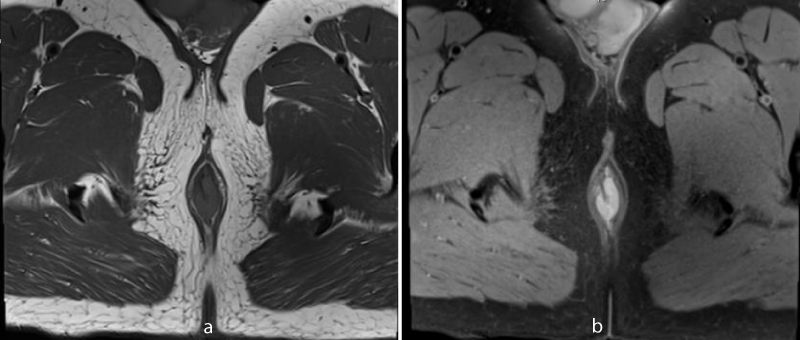
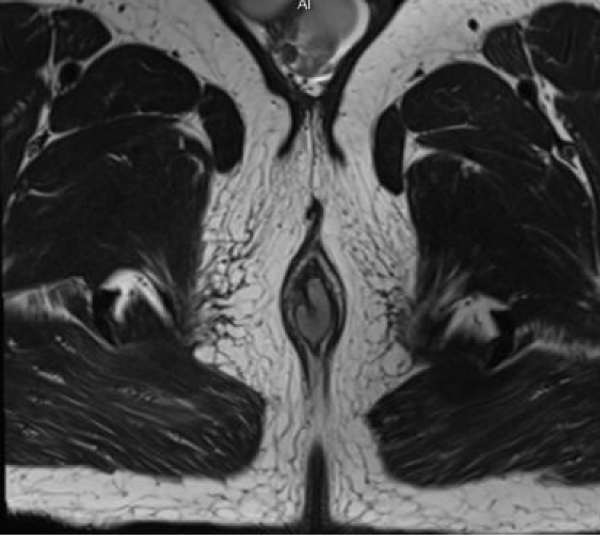
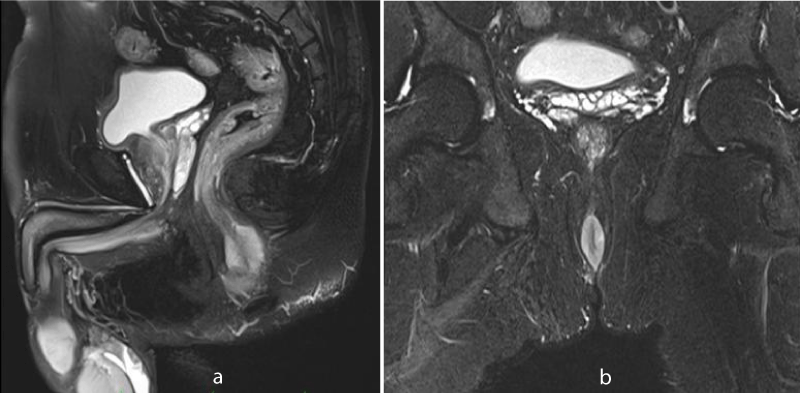
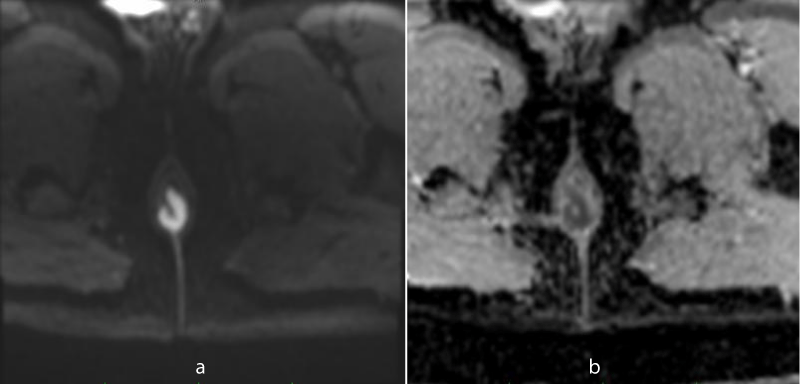
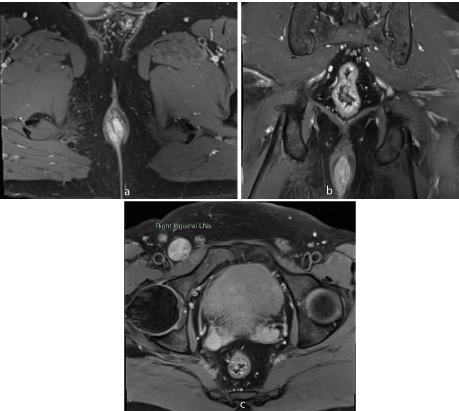
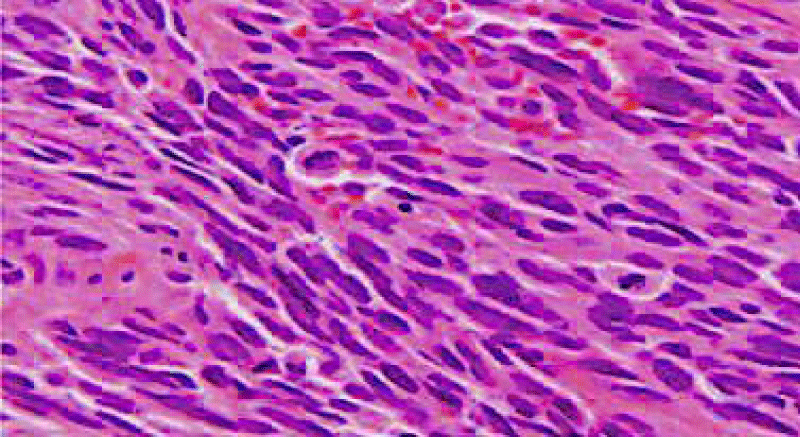
MR imaging revealed short segment circumferential wall thickening of the anal canal with lower margin approximately 1.7cm from anal verge. It was nearly 3 cm in length and 7mm in maximum thickness. The wall thickening showed hyperintense signal in T1-weighted images and T2-weighted images (Figures 1-3). Restricted diffusion with corresponding low signal in ADC map was noted figure 4. Post gadolinium T1-weighted fat saturated images showed hyper enhancement of the wall thickening (Figure 5). The thickening was involving the internal sphincter. No invasion of intersphincteric plane and external sphincter was noted. No extension into perianal fat was noted. Few enlarged heterogenously enhancing lymph nodes were noted in right inguinal region largest 23 x 21 mm in size. The patient underwent wide local excision with right inguinal dissection and adjuvant loco-regional radiotherapy. The histopathological examination showed features suggestive of primary anal malignant melanoma (Figure 6). In routine follow up, the patient showed no features of local recurrence or distant metastasis.
Figure 1: 60 year old male with primary anal melanoma. Axial T1-weighted MR image without fat saturation (a) and with fat saturation (b) shows circumferential hyperintense wall thickening in anal canal.
Figure 2: Axial T2-weighted MR image also shows hyperintense signal of the wall thickening.
Figure 3: Sagittal (a) and coronal (b) T2-weighted fat saturated MR image shows hyperintense signal of anal canal wall thickening.
Figure 4: Restricted diffusion is seen in DW image (a) with corresponding low signal in ADC map (b).
Figure 5: Axial (a) and coronal (b) post gadolinium T1-weighted fat saturated MR image shows enhancing wall thickening and associated right inguinal lymphadenopathy (c).
Figure 6: Hematoxylin and eosin stain shows marked nuclear pleomorphism, abnormal mitotic activity and melanin pigment, 10x.
Malignant melanoma of the anal canal is a rare disease. The incidence is approximately 0.4% - 3.0% of all malignant melanomas and 0.1% - 4.6% of all anorectal malignant tumors [1-3]. The malignancy affects the anal canal, the rectum or both with majority occurring within 6 cm of the anal verge [4]. It arises at or above the dentate line in 52% - 92% of cases and rectal in 2% - 5% of cases [5]. Moore reported the first case of melanoma of anus and rectum in literature in 1857 [6]. The peak incidence is seen in the sixth and seventh decades. The patients present with pain, anal mass, bleeding per rectum, tenesmus or change in the bowel habits [7]. The clinical symptoms of anal melanoma are misdiagnosed in about two thirds of patients as haemorrhoids, skin tag or polyp [8].
Anal melanoma presents as intraluminal polypoid mass or circumferential wall thickening with minimal perianal infiltration and absence of colonic obstruction. A retrospective study to evaluate MRI features in 12 patients of pathologically proven primary anorectal melanoma was done. MRI scans revealed 11 lesions and one lesion could not be detected on MRI. The lesions were seen as intraluminal polypoid mass in 9 patients and intraluminal ulcerated polypoid mass in 2 patients. None of the lesions had an exophytic shape or showed wall thickening [9]. Another retrospective study evaluating computed tomographic (CT) findings in 8 patients with pathologically proven primary malignant melanoma of the rectum showed polypoid or fungating intraluminal mass as the most common finding [10]. The patient in our case showed circumferential wall thickening which is an uncommon finding in primary anal malignant melanoma. The melanotic component shows hyperintense signal in T1-weighted images and hyperintense or mixed signal in T2-weighted images [11]. High signal intensity in Diffusion weighted images with corresponding low signal in ADC map and post contrast hyperenhancement is also noted. Associated lymphadenopathy in perirectal, internal iliac, obturator and inguinal regions can be present. These findings help to differentiate primary anal malignant melanoma from adenocarcinoma, the most common malignancy of the anorectum. Anorectal adenocarcinoma commonly presents as an infiltrative ulcerative mass that causes significant luminal narrowing and proximal bowel obstruction because of its desmoplastic stroma. MRI findings of adenocarcinoma are hypointense signal in T1-weighted images and hyperintense signal in T2-weighted images.
The anorectal melanoma has the tendency for submucosal infiltration. The submucosal spread predisposes to lymph node metastases in 44% of cases [5]. Distant metastases are present in upto 90% of cases with lymph node involvement [12]. Thus, it is mostly unrespectable at the time of diagnosis [13]. Clinical staging of anal melanoma is based on locoregional and distant spread. Stage I is local disease, stage II is local disease with regional lymphadenopathy and stage III is distant metastatic disease [14]. The most common sites for distant metastases are inguinal lymph nodes, mesenteric lymph nodes, hypogastric lymph nodes, para-aortic lymph nodes, liver, lung, skin, and brain. The 5-year survival rate can range from 16% to 34% in patients diagnosed with anorectal melanoma [13].
Surgical resection remains the mainstay of treatment. The optimal surgical procedure for primary malignancy is controversial and vary from sphincter sparing wide local excision to abdominoperineal resection requiring a permanent colostomy. Surgery also plays a significant role in palliative care and management of locally recurrent disease. Since, majority of patients are diagnosed at late stages of the malignancy, curative excision is not possible in such patients. The mean survival of patients with anorectal melanoma after treatment is 20 months and there are no long term survivors among patients with stage II and stage III disease [14,15].
Chemotherapy and radiation therapy alone are not effective, however may be useful when used in an adjuvant fashion. Dacarbazine is the most commonly used single agent and around 20% of patients show a partial response in 4-6 months after treatment [14]. Lens and Dawes conducted randomized controlled trials comparing regimens with and without interferon α, however no definite conclusion was drawn regarding its efficacy in the treatment of anal melanoma [16]. Ulmer, et al. employed intratumoral injections of interferon β and systemic dacarbazine leading to significant reduction in size of local tumor [17]. Studies show that wide local excision and adjuvant loco-regional radiotherapy result in comparable control of the disease with less loss of function compared to abdominoperineal resection [18].
Primary anal malignant melanoma is a rare, highly aggressive malignancy with poor prognosis. Anal melanoma presents as intraluminal polypoid mass or circumferential wall thickening with minimal perianal infiltration and absent proximal bowel obstruction. MRI findings include hyperintense signal in T1-weighted images and hyperintense/mixed signal in T2-weighted images, restricted diffusion and post contrast hyperenhancement which differentiate the anal melanoma from other anorectal lesions. Surgery remains the mainstay of treatment, however the optimal procedure is still controversial. Adjuvant chemotherapy, interferon and radiation may offer some benefit. The only hope of improved life expectancy is early diagnosis and treatment.
- Heyn J, Placzek M, Ozimek A, Baumgaertner AK, Siebeck M, et al. Malignant melanoma of the anal region. Clin Exp Dermatol. 2007; 32: 603–607.
- Chang AE, Karnell LH, Menck HR. The National cancer data base report on cutaneous and noncutaneous melanoma: a summary of 84836 cases from the past decade. Cancer. 1998; 83: 1664-1678. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9781962
- Klas JV, Rothenberger DA, Wong WD, Madoff RD. Malignant tumors of the anal canal: the spectrum of disease, treatment and outcomes. Cancer. 1999; 85: 1686-1693. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10223561
- Zhang S, Gao F, Wan D. Effect of misdiagnosis on the prognosis of anorectal malignant melanoma. J cancer Res Clin Oncol. 2010; 136: 1401-1405. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20130908
- Falch C1, Stojadinovic A, Hann-von-Weyhern C, Protic M, Nissan A, et al. Anorectal malignant melanoma: extensive 45 year review and proposal for a novel staging classification. J Am Coll Surg. 2013; 217: 324-335. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23697834
- Moore R. Recurrent melanosis of the rectum, after previous removal from the verge of the anus, in a managed sixty five. Lancet. 1857; 1: 290.
- Saraswat B, Purohit R, Singh A, Yadav R. Primary anal malignant melanoma: a case report. Int Surg J. 2015; 2: 304-307.
- Felz MW, Winburn GB, Kallab AM, Lee JR. Anal melanoma: an aggressive malignancy masquerading as haemorrhoids. South Med J. 2001; 94: 880-885. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11592745
- Park HJ, Kim HJ, Park SH, Lee JS, Kim AY, et al. Primary anorectal melanoma: MRI findings and clinicopathological correlations. AJR. 2018; 211: 98-108. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29927334
- Kim KW, Ha HK, Kim AY, Kim TK, Kim JS, et al. Primary malignant melanoma of the rectum: CT findings in eight patients. Radiology. 2004; 232: 181-186. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15220501
- Matsuoka H, Nakamura A, Iwamoto K, Sugiyama M, Hachiya J, et al. Anorectal malignant melanoma: Preoperative usefulness of magnetic resonance imaging. J Gastroenterol. 2005; 40: 836–842. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16143890
- Kelly P, Zagars GK, Cormier JN, Ross MI, Guadagnolo BA. Sphincter sparing local excision and hypofractionated radiation therapy for anorectal melanoma: a 20 year experience. Cancer. 2011; 117: 4747-4755. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21446049
- Stefanou A, Nalamati SP. Anorectal melanoma. Clin Colon Rectal Surg. 2011; 24: 171-176. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22942799
- Singer M, Mutch MG. Anal melanoma. Clin Colon Rectal Surg. 2006; 19: 78–87. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20011314
- Yap LB, Neary P. A comparison of wide local excision with abdominoperineal resection in anorectal melanoma. Melanoma Res. 2004; 14: 147-150. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15057046
- Lens MB, Dawes M. Interferon therapy for malignant melanoma: a systemic review of randomized controlled trials. J Clin Oncol. 2002; 20: 1818-1825. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11919239
- Ulmer A, Metzger S, Fierlbeck G. Successful palliation of stenosing anorectal melanoma by intratumoral injections of natural interferon β. Melanoma Res. 2002; 12: 395-398. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12170190
- van Schaik PM, Ernst MF, Meijer HA, Bosscha K. Melanoma of the rectum: A rare entity. World J Gastroenterol. 2008; 14: 1633–1635. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2693766/