More Information
Submitted: December 08, 2020 | Approved: December 21, 2020 | Published: December 22, 2020
How to cite this article: Ganta R, Kantharia SR, Shah BB, Vasava RM, Vaishnav TV, et al. Role of HRCT Thorax in pre-operative assessment of RT-PCR COVID-19 negative oral cancer patients. J Radiol Oncol. 2020; 4: 008-011.
DOI: 10.29328/journal.jro.1001033
Copyright License: © 2020 Ganta R, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: COVID-19; HRCT Thorax; Oral cancer; RT-PCR
Role of HRCT Thorax in pre-operative assessment of RT-PCR COVID-19 negative oral cancer patients
Roopa Ganta1, Shehnaz R Kantharia2, Bhavin Bhupendra Shah3, Rajinikant Mohan Vasava3, Tushar Vishnuprasad Vaishnav3 and Rajesh A Kantharia4*
1Department of Head and Neck Oncology, Kailash Cancer Hospital and Research Centre, Muniseva Ashram, Goraj, Waghodia. 391761, Baroda, Gujarat, India
2Department of Clinical Research and Consultant Otorhiynolaryngology and Head and Neck Oncology, Kailash Cancer Hospital and Research Centre, Muniseva Ashram, Goraj, Waghodia. 391761, Baroda, Gujarat, India
3Department of Radiology, Kailash Cancer Hospital and Research Centre, Muniseva Ashram, Goraj, Waghodia. 391761, Baroda, Gujarat, India
4Department of Head and Neck Oncology, Kailash Cancer Hospital and Research Centre, Muniseva Ashram, Goraj, Waghodia. 391761, Baroda, Gujarat, India
*Address for Correspondence: Dr. Rajesh A Kantharia, MBBS, MS, Fellowship Head and Neck Oncosurgery (Tata Memorial Hospital), Medical Director and Head of Department, Head and Neck Oncosurgery, Kailash Cancer Hospital and Research Center, Muniseva Ashram, Goraj, Waghodia, 391760 Baroda, Gujarat, India, Tel: 02668-265413; 9825860896; Email: [email protected]
Background: Oral cancer accounts for 30% of all types of cancer in India. Surgery is the mainstay of treatment but due to the recent outbreak of COVID-19, there is a partial or complete disruption of health services in the country. The initial delay in the treatment was due to cancellations of planned surgeries as per government regulations and reduction in public transportation. In the latter half of the initial relaxation of the lockdown, we formulated our institutional protocol for the surgical treatment of oral cancer patients. On admission, all patients were kept in isolated wards followed by RT-PCR (Reverse Transcriptase-Polymerase Chain Reaction) testing on the same day. RT-PCR negative patients are subjected to HRCT Thorax (High-resolution Computer Tomography). This ensured the safety of health care workers, patients, and patient attendees. Keeping this in mind, we did an observational study on the role of HRCT in the pre-operative screening of asymptomatic oral cancer patients.
Materials and methods: Retrospective analysis of prospectively collected data of 150 patients was done. HRCT reporting was done by two experienced senior radiologists of the Department of Radiology at our hospital.
Results: The number of patients under the CO-RADS 1 category was 121 and CO-RADS 2 category was 29, according to CO-RADS classification. The results of RT-PCR and HRCT were compared and there was a 100% positive correlation between RT-PCR and HRCT Thorax.
Conclusion: Our study supported the use of HRCT Thorax as a diagnostic tool in pre-operative screening of oral cancer patients for COVID 19, particularly in RT-PCR negative cases.
The recent outbreak of coronavirus (COVID-19) was declared a global pandemic on 11th March by WHO with the first patient identified in Wuhan, China [1]. As of June 30th, 2020, around 5 million cases of COVID-19 have been reported in 188 countries and has resulted in more than 452000 deaths [1,2]. India, a country of 1.35 billion people, has also come in the grasp of this highly contagious disease with its first case reported on 30 January in the state of Kerala [3]. The Government of India on 24th March 2020, ordered a nationwide lockdown for 21 days (till April’15), by limiting movement of the entire 1.3 billion population of India as a preventive measure against the COVID-19 pandemic in India [5].
The health care system is trying to fight the new coronavirus, the threat of more people dying of other health conditions like cancer is alarmingly large [4]. In China, analysis has shown that the case fatality rate in cancer patients is 3.5 times more than seen in non-cancer patients [6]. According to data from the WHO, more than 2000 patients die every day due to cancer in India. So, an additional waiting period for surgery and subsequent adjuvant treatment would prove to be fatal for many. In India, oral cancer accounts for 30% of all types of cancer most with squamous histology and having an advanced stage on presentation [7]. Curative surgery and primary reconstruction are the mainstays of treatment for these locally advanced oral cancers. Operating on these patients presents us with a considerable risk of a high viral load while operating in the oral cavity and exposure to the aerosol generated during a 3-4 hours surgery.
During this lockdown, we realized that confinement of COVID-19 is critical, but curative treatment of cancer should not be ignored. During the lockdown, there was an initial delay in the treatment for 2-3 weeks and this was due to the time taken to set institutional protocols, train the staff about the basics of social distancing, usage of PPE kits, and new methods of sanitization and sterilization. During 1st phase lockdown, as there was cancellation of planned surgeries as per government regulations, we prepared a list of patients waiting for surgery and started planned surgeries form April’15. During this time there were no standard guidelines proposed by regional/national cancer associations or by the Indian Medical Association. Protection of our staff, judicious use of available resources, and a rational and balanced attitude towards cancer patients was the need of the hour. In the Department of Head and Neck Oncology, we formulated our protocol for the surgical treatment of oral cancer patients in this pandemic. The protocol included indoor admission of the patient 2 days before surgery for preoperative COVID 19 work up in the form of RT-PCR (Real-Time Polymerase Chain Reaction) and HRCT Thorax(High-Resolution Computer Tomography). With our formulated protocol we continued working during the lockdown and extended lockdown offering curative surgery for our Oral cancer patients also ensuring the safety of our staff, patients, and attendees.
The Real-time Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) test is the definitive test for COVID-19. It is highly specific with a reported sensitivity of 60% - 70% [8]. Thus, false negatives are a real clinical problem. HRCT Thorax for COVID-19 has high sensitivity, can be performed faster and when used in conjunction with RT-PCR the combined specificity and sensitivity for COVID-19 is up to 90%.
Given this, our Head and Neck Oncology Department conducted an observational study on the role of HRCT Thorax in the preoperative screening of asymptomatic oral cancer patients during the COVID-19 pandemic.
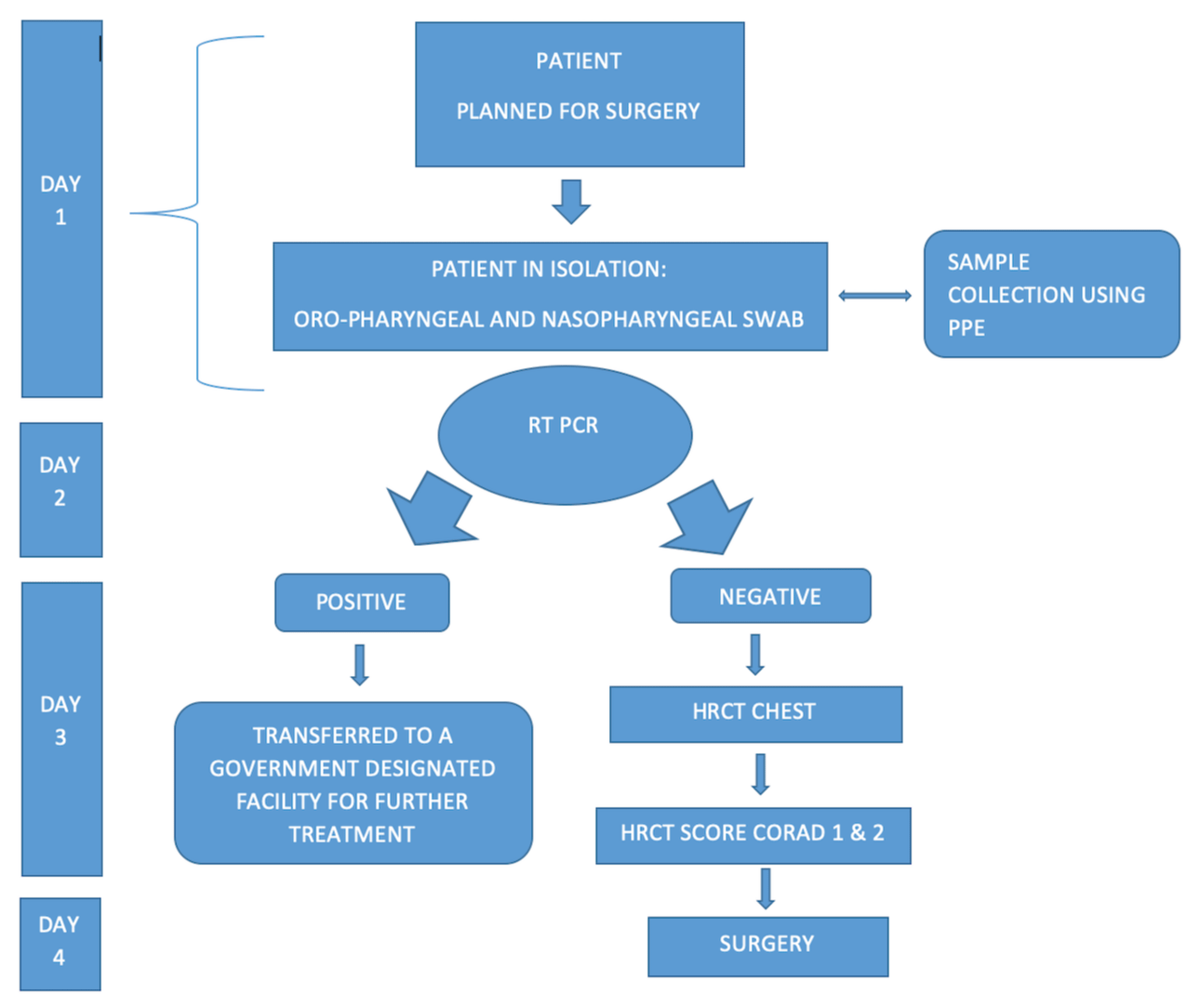
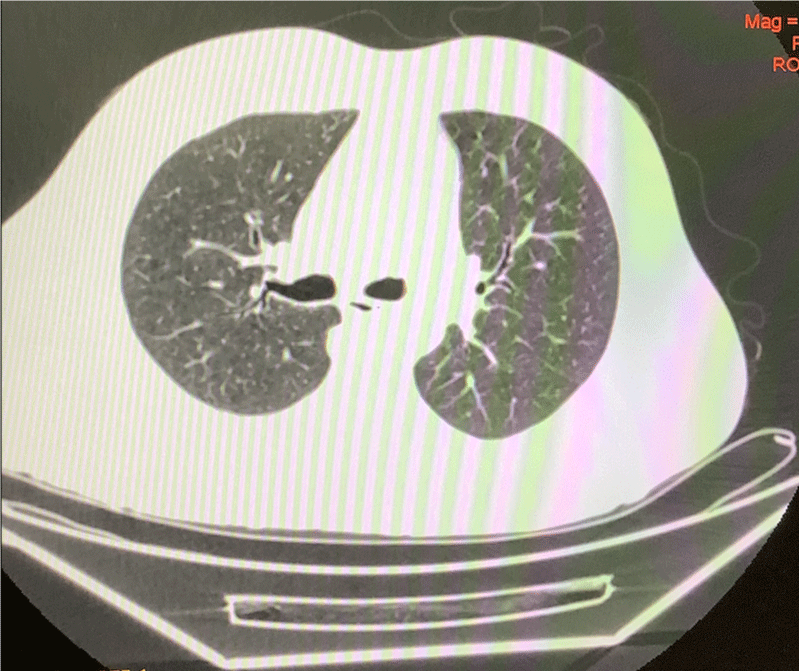
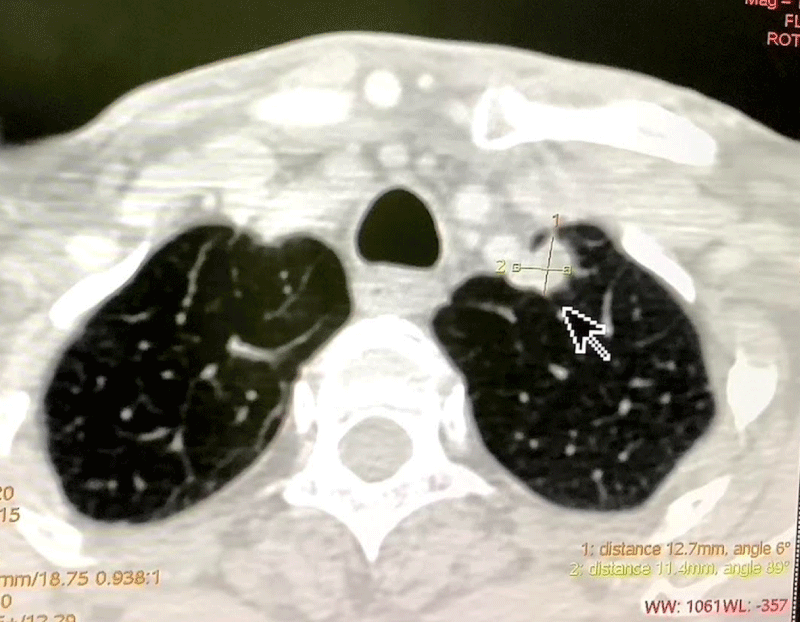
Our data of 150 pre-operative Oral Cavity Squamous Cell Carcinoma patients from 15th April to 31st July was analyzed. The patients were admitted 2 days before the date of surgery for initial assessment by RT-PCR testing. The patients with a negative RT PCR report were then subjected to HRCT Thorax and only if there were no signs suggestive of a COVID-19 infection on the HRCT scan as well, the patients were taken up for surgery. Based on the CT findings, the level of suspicion of COVID-19 infection was graded using CO-RADS classification (Table 1) (Figures 2,3). The detection rate of COVID-19 infection based on the initial RT-PCR and HRCT Thorax was compared (Figure 1). The purpose of study was explained and informed consent has been taken from patient. The ethical clearance was obtained from ethical subcommittee of institute before commencement of study.
| Table 1: CO-RADS Classification. | ||
| CO-RADS | Level of Suspicion for COVID-19 | Ct Findings |
| CO-RADS 1 | No | Normal Or non-infectious etiology |
| CO-RADS 2 | Low | Abnormalities Consistent with infections other than COVID-19 |
| CO-RADS 3 | Indeterminate | Unclear whether COVID-19 is present |
| CO-RADS 4 | High | Abnormalities suspicious for COVID-19 |
| CO-RADS 5 | Very High | Typical COVID-19 |
| CO-RADS 6 | PCR + | |
Figure 1: Flow chart (Depicting the sequential steps prior to surgery).
Figure 2: HRCT Thorax (CO-RADS 1) No abnormality detected.
Figure 3: HRCT Thorax (CO-RADS 2): Left apical segment nodular opacity 12.7 x 11.4 mm.
The RT-PCR assays were performed by using Real-Time PCR by Applied Biosystems TaqpathTM COVID-19 Combo kit from Unipath laboratory Ltd, Baroda Gujarat.
Imaging analysis was done by two senior radiologists at our hospital in the Department of Radiology. They reviewed all HRCT Thorax images and classified them based on CO-RADS Classification. The CT scan used was GE 16 SLICE CT SCANNER with all scans done with patients in the supine position. The statistics was done by simple percentage analysis.
A total of 150 patients were included (108 male, 42 female) with a mean age of 49.82 years (range 21-81 years). For all the patients, an initial assessment with RT-PCR testing was done. The patients with the negative report were subjected to HRCT Thorax. Based on the CT findings, the level of suspicion of COVID-19 infection was graded using the CO-RADS classification. Imaging analysis was done by two experienced senior radiologists at our hospital. The number of patients under CO-RADS 1 category was 80.66% (121/150) and CO-RADS 2 category in 19.33% (29/150) as shown in table 2, according to CO-RADS classification.
| Table 2: CO-RADS, level of suspicion for COVID-19 infection. | |
| CO-RADS | No of patients |
| CO-RADS 1: | 121 |
| CO-RADS 2: | 29 |
Among 150 patients, 60% (90/100) patients had no abnormalities on HRCT(CO-RADS 1) and in 40% (60/100) there were minor abnormalities (CORADS 1,2) not related to COVID-19 infection such as fibrocalcific changes in 13.33% (20/150) which are due to the past history of Tuberculosis, atelectasis in 4% (6/150) due to old age, lung disease such as asthma, COPD, and emphysema related changes in 2% (3/150) due to history of smoking. Soft tissue nodules in 2.6% (4/150), non-calcific nodules in 0.6% (1/150), cyst in 4% (6/150), nodular opacity in 6% (9/150), Mediastinal lymph nodes in 2.6% (4/150), cylindrical bronchiectatic changes in 1.3% (2/150), centrilobular nodule in 1.3% (2/150), subpleural nodules in 2% (3/150) of patients correlates to infective aetiology (Table 3).
| Table 3: HRCT details of minor abnormalities not related to COVID-19 infection. | ||
| HRCT details | No. of patients | CO-RADS |
| Fibrocalcific changes and calcific nodules | 20 | CO-RADS 1 |
| Atelectasis | 6 | CO-RADS 1 |
| Emphysema | 3 | CO-RADS 1 |
| Soft tissue nodules | 4 | CO-RADS 2 |
| Non-calcific nodules | 1 | CO-RADS 2 |
| Sub-pleural nodules | 3 | CO-RADS 2 |
| Cyst | 6 | CO-RADS 2 |
| Nodular opacity | 9 | CO-RADS 2 |
| Mediastinal lymph nodes | 4 | CO-RADS 2 |
| Cylindrical brochiectatic changes | 2 | CO-RADS 1 |
| Centrilobular nodules | 2 | CO-RADS 2 |
| Total | 60 | |
HRCT Thorax is a conventional, non-invasive imaging modality with high accuracy and speed. In recent literature, based on available data, almost all patients with COVID-19 had characteristic CT features in the disease process, such as different degrees of ground-glass opacities with/without crazy-paving sign, multifocal organizing pneumonia, and architectural distortion in a peripheral distribution [9,10].
In our study, CT Thorax was done in RT-PCR negative oral cancer patients. Several studies were determining the sensitivity of CT Thorax in comparison with RT-PCR and the role of CT Thorax in the COVID-19 situation.
A study was conducted by Ai Tao, et al. to investigate the diagnostic value and consistency of chest CT as compared with comparison to RT-PCR assay in COVID-19. The study includes 1014 patients who underwent both chest CT and RT-PCR tests. Among 1014 patients, 59% (601/1014) had positive results for RT-PCR, and 88% (888/1014) had positive results for chest CT scans. Based on positive RT-PCR results, the sensitivity of chest CT in suggesting COVID-19 was 97% (95% CI, 95% - 98%, 580/601 patients). And 75% (308/413) patients had positive chest CT findings with negative RT-PCR results. They have concluded that Chest CT has a high sensitivity for the diagnosis of COVID-19 [9]. This is consistent with our study.
In a study by Fang, et al. on the Sensitivity of chest CT for COVID-19 in comparison to RT- PCR have concluded that the sensitivity of chest CT in COVID-19 was higher than that of RT- PCR (98% vs. 71%, respectively) [11].
Keeping all this in mind we formulated a protocol to ensure the safety of the hospital staff, patients, and the attendees. In our study of 150 cases, there was a 100% positive correlation between the results of RT-PCR and CT Thorax. All RT-PCR negative patients showed no signs of COVID-19 on HRCT Thorax.
Our study supported the use of HRCT Thorax as a diagnostic tool in pre-operative screening of oral cancer patients for COVID 19, particularly in RT-PCR negative cases.
- Del Rio C, Malani PN. COVID‐19-New insights on a rapidly changing epidemic. JAMA. 2020; 323: 1339-1340. PubMed: https://pubmed.ncbi.nlm.nih.gov/32108857/
- WHO. Statement on the Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019‐nCoV). Geneva, Switzerland: WHO Newsletter; 2020.
- India's First Coronavirus Case: Kerala Student in Wuhan Tested Positive. Chennai, India: Business Standard News: 2020.
- www.deccanherald.com
- en.wikipedia.org
- Liang W, Guan W, Chen R, Wang W, Li J, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020; 21: 335-337. PubMed: https://pubmed.ncbi.nlm.nih.gov/32066541/
- Sankaranarayanan R, Ramadas K, Thomas G, Muwonge R, Thara S, et al. Effect of screening on oral cancer mortality in Kerala, India: a cluster- randomised controlled trial. Lancet. 2005; 365: 1927–1933. PubMed: https://pubmed.ncbi.nlm.nih.gov/15936419/
- Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. Essentials for Radiologists on COVID-19: An Update—Radiology Scientific Expert Panel. Radiology. 2020; 296: E113-E114. PubMed: https://pubmed.ncbi.nlm.nih.gov/32105562/
- Ai T, Yang Z, Hou H, Zhan C, Chen C, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020; 96: E32-E40. PubMed: https://pubmed.ncbi.nlm.nih.gov/32101510/
- Shi H, Han X, Jiang N, Cao Y, Alwalid O, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020; 20: 425-434.
- Fang Y, Zhang H, Xie J, Lin M, Ying L, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020; 296: E115-E117. PubMed: https://pubmed.ncbi.nlm.nih.gov/32073353/