More Information
Submitted: May 26, 2023 | Approved: June 19, 2023 | Published: June 20, 2023
How to cite this article: Calixte A, Lartigue S, McGaugh S, Mathelier M, Patel A, et al. Neurointerventional Radiology: History, Present and Future. J Radiol Oncol. 2023; 7: 026-032.
DOI: 10.29328/journal.jro.1001049
Copyright License: © 2023 Calixte A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Neurointerventional radiology (NIR); Endovascular neurosurgery; Interventional neurology; Cerebrovascular surgery; Endovascular treatment; Minimally invasive therapies
Neurointerventional Radiology: History, Present and Future
Andre Calixte1*, Schan Lartigue1, Scott McGaugh2, Michael Mathelier2, Anjali Patel2, Mohammad Reza Hosseini Siyanaki3, Kevin Pierre4 and Brandon Lucke-Wold3
1New York Medical College, Valhalla, New York, 10595, USA
2University of Florida College of Medicine, Gainesville, Florida, 32608, USA
3University of Florida Department of Neurosurgery, Gainesville, Florida, 32608, USA
4University of Florida Department of Radiology, Gainesville, Florida, 32608, USA
*Address for Correspondence: Andre Calixte, New York Medical College, Valhalla, New York, 10595, USA, Email: [email protected]
Neurointerventional Radiology (NIR), encompassing neuroendovascular surgery, endovascular neurosurgery, and interventional neurology, is an innovative and rapidly evolving multidisciplinary specialty focused on minimally invasive therapies for a wide range of neurological disorders. This review provides a comprehensive overview of NIR, discussing the three routes into the field, highlighting their distinct training paradigms, and emphasizing the importance of unified approaches through organizations like the Society of Neurointerventional Surgery (SNIS).
The paper explores the benefits of co-managed care and its potential to improve patient outcomes, as well as the role of interdisciplinary collaboration and cross-disciplinary integration in advancing the field. We discuss the various contributions of neurosurgery, radiology, and neurology to cerebrovascular surgery, aiming to inform and educate those interested in pursuing a career in neurointervention. Additionally, the review examines the adoption of innovative technologies such as robotic-assisted techniques and artificial intelligence in NIR, and their implications for patient care and the future of the specialty.
By presenting a comprehensive analysis of the field of neurointervention, we hope to inspire those considering a career in this exciting and rapidly advancing specialty, and underscore the importance of interdisciplinary collaboration in shaping its future.
Neurointerventional Radiology (NIR), also known as neuroendovascular surgery, endovascular neurosurgery, or interventional neurology, is an innovative and rapidly evolving specialty that combines the expertise of multiple disciplines to provide minimally invasive therapies for a wide range of neurological disorders.
History of neurointerventional radiology
The origins of NIR date back to the 1960s and 1970s, with the development of selective angiography and the introduction of endovascular therapies for the treatment of neurological disorders. Since then, the field has experienced significant advancements in imaging technology, materials, and procedural techniques, leading to an expansion in its scope and capabilities. Today, NIR encompasses a variety of interventions, such as endovascular treatment of cerebral aneurysms, arteriovenous malformations, stroke management, and carotid artery stenting.
The field’s early days can be traced back to the pioneering work of Portuguese neurologist Egas Moniz, who, with Pedro Almeida Lima, developed the first cerebral angiogram in 1920. This technique revolutionized the visualization of cerebral tumor vascular supply and was widely used until being replaced by the advent of Computed Tomography (CT) scans [1,2].
The first minimally invasive endovascular treatment of an intracranial aneurysm was performed in 1939. Gerard Debrun, regarded as the father of interventional neuroradiology, developed a detachable latex balloon catheter to treat carotid cavernous fistulae and giant intracavernous aneurysms [3,4]. This technique was quickly adopted for its novelty and efficiency. In 1990, neurosurgeon Guido Guglielmi introduced a new method to treat intracranial aneurysms using detachable coils [4,5]. The International Subarachnoid Aneurysm Trial in 2005 compared endovascular versus open surgical treatments, demonstrating better independent survival odds and lower morbidity and mortality with endovascular coiling. These findings persisted in the 5-year follow-up, making endovascular coiling a preferred treatment method for ruptured intracranial aneurysms [6].
The Prolyse in Acute Cerebral Thromboembolism (PROACT II) trial revealed increased rates of recanalization and functional independence in patients receiving intra-arterial thrombolysis for acute middle cerebral artery occlusion [7]. Additionally, the MR CLEAN study demonstrated the efficacy and safety of intra-arterial thrombolysis for acute ischemic strokes caused by proximal occlusion in the anterior circulation. IAT led to a 10% absolute reduction in poor outcomes after stroke [8].
Further trials, such as DAWN, DEFUSE 3, and MR RESCUE, highlighted the advantages of mechanical thrombectomy for ischemic strokes, leading to the incorporation of this technique into standard treatment and the relaxation of eligibility criteria. These studies showcased the therapeutic benefits of NIR techniques, offering patients improved chances of recovery and functional independence [9-11]. As advances continue, trials assessing the efficacy and safety of endovascular treatments for ischemic strokes have shown that patients significantly benefit from the integration of neuroendovascular approaches, with some studies even extending the critical window for intervention up to 24 hours [12,13].
Neurointerventional radiology today
Today, NIR is at the forefront of numerous innovative techniques used for treating central nervous system (CNS) pathologies. The growing demand for comprehensive stroke centers, along with the overall expansion of NIR, has led to an increased need for skilled neurointerventional practitioners.
Among the neurointerventional procedures currently available are diagnostic angiograms, dural venous pressure measurements, inferior petrosal sinus sampling, Wada testing, and various neck and spinal diagnostic procedures, including myelography, cisternography, image-guided lumbar puncture, and vertebral biopsy. Therapeutic procedures feature aneurysm coiling, flow diversion stenting, carotid artery stenting, intracranial and spinal arteriovenous fistula embolization, vein of Galen malformation embolization, balloon-assisted endovascular embolization, middle meningeal artery embolization, epistaxis embolization, tumor embolization (e.g., meningiomas and lingual carcinomas), arterial and venous mechanical thrombectomy, venoplasty, venous stenting, arterial angioplasty, and intra-ophthalmic artery chemotherapy [14-19].
Pathways into neurointervention
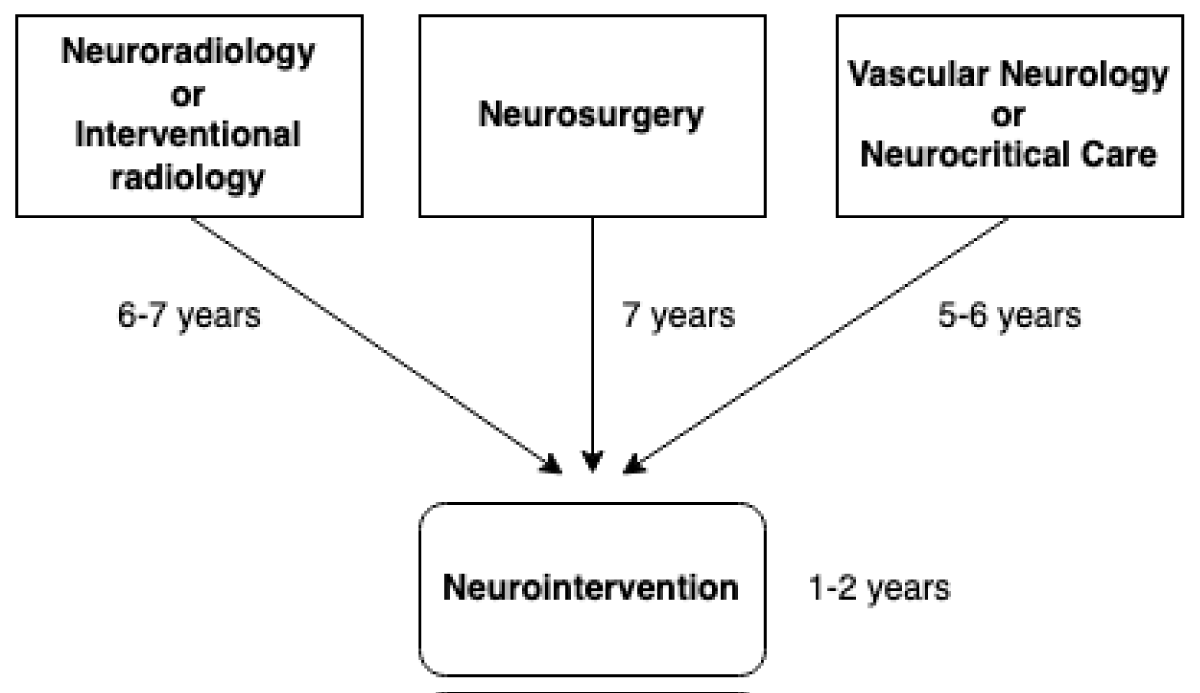
In the United states, there are three primary pathways to becoming a neurointerventionalist: neurosurgery, radiology, and neurology as outlined by the SNIS (Figure 1). Each pathway offers unique perspectives, training experiences, and opportunities for professional development [20,21].
Figure 1: Neurointerventional training pathways based on primary specialty as outlined by the SNIS.
Neurosurgery is a surgical specialty centered on the diagnosis and management of CNS disorders, including the brain and spine. The pathway to becoming a neuro-interventionalist through neurosurgery typically involves completing a 7-year neurosurgical residency followed by a 1-2 year fellowship in endovascular neurosurgery or interventional neuroradiology. Enfolded fellowships are often performed within residency, followed by 1 year of training in endovascular neurosurgery. The unique strength of this route is the combination of an extensive surgical background with interventional techniques, providing expertise in managing complex cases requiring both open and endovascular approaches. Furthermore, complications arising during a procedure can be addressed through immediate conversion to open surgery [4,21-25].
Radiology offers a diagnostic perspective, emphasizing medical imaging techniques and image interpretation. To become a neurointerventionalist via the radiology route, one must complete a preliminary internship year, 4-year diagnostic radiology residency and then a neuroradiology fellowship, usually lasting 1-2 years, followed by additional training in interventional neuroradiology. Alternatively, an integrated interventional radiology residency, which typically takes 5 years following the completion of a preliminary internship year, can be completed followed by training in interventional radiology. The unique strength of this pathway lies in the mastery of catheter skills acquired during training and the thorough understanding of diagnostic imaging’s applications, which guide the planning and execution of neurointerventional procedures effectively [21,26].
Lastly, neurology focuses on the diagnosis and non-surgical management of neurological disorders. Trainees with a neurology background possess extensive clinical skills and a deep understanding of the natural progression of vascular pathologies. The pathway to NIR through neurology requires a 4-year neurology residency, followed by a 1-2 year vascular neurology/stroke or neurocritical care fellowship, and additional training in interventional neuroradiology. Neurologists bring a thorough understanding of the medical aspects of neurological diseases, which can be invaluable in assessing and managing patients before, during, and after neurointerventional procedures [21,27].
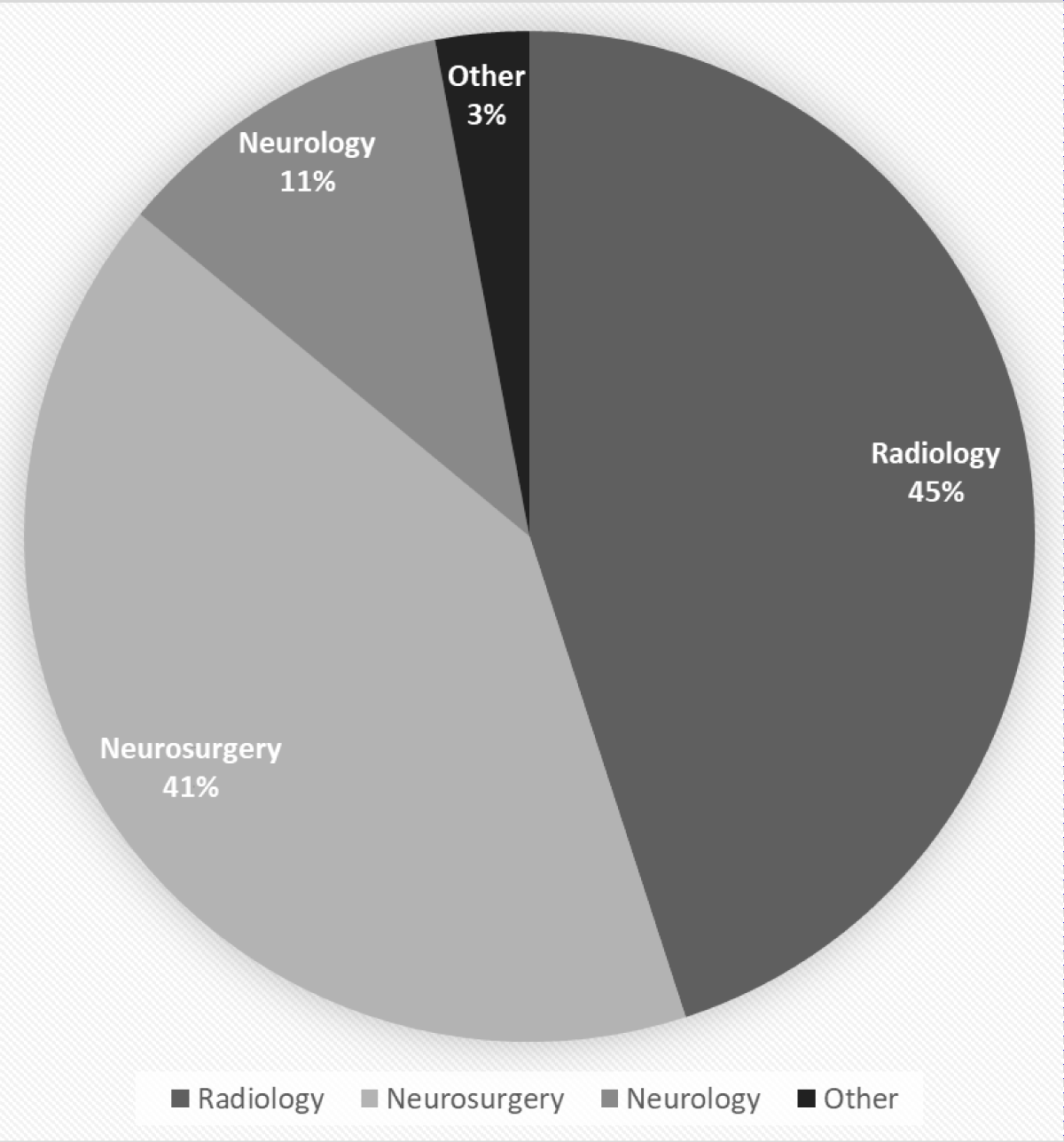
In Figure 2, Cox, et al. demonstrate the approximate distribution of neurointerventionalists by primary specialty using data adapted from [28]. Other specialties may contribute to NIR procedures. For example, orthopedic surgeons contribute significantly to percutaneous spine procedures. Cardiologists and vascular surgeons often perform carotid endarterectomies. The distribution is similar in Canada, with 52% being neuroradiologists, 38% neurosurgeons, and 9% neurologists [29].
Figure 2: The percentage of each specialty that performed intracranial endovascular procedures in 2016. Data adapted from [28].
Specialty integration
To further enhance collaboration and advance the field of neurointervention, a unified approach that leverages the strengths of organizations, joint conferences, online platforms, and continuing education is crucial. By adopting such a comprehensive strategy, professionals from various backgrounds can share their knowledge, experiences, and ideas, thereby fostering innovation and improving patient care.
Organizations such as the Society of NeuroInterventional Surgery (SNIS) play a pivotal role in bringing together professionals from diverse backgrounds, including neurosurgery, neuroradiology, and neurology [30]. SNIS provides a platform for these specialists to collaborate on research, share best practices, and develop guidelines for patient care. Variability in recommendations among specialties is a concern, as clinicians from different specialties may have different approaches to patient care [31]. Organizations such as SNIS allow for standardization of guidelines between organizations and specialties. Moreover, by facilitating interaction and cooperation among its members, and providing opportunities for joint training and learning, SNIS ensures that the latest advancements in neurointerventional techniques and therapies are disseminated across the field.
Joint conferences represent another valuable opportunity for collaboration. These events allow attendees to exchange ideas, present research findings, and discuss new develop-ments in the field of neurointervention. By hosting sessions and workshops that cater to various backgrounds and skillsets, joint conferences provide an inclusive environment that encourages the development of interdisciplinary relationships and mentorship.
In addition, online platforms have become increasingly important in promoting communication and collaboration in the field of neurointervention. These platforms include forums, webinars, social media, and virtual conferences, which offer opportunities for professionals to connect and share their expertise. By leveraging these digital resources, specialists can keep up-to-date with the latest advancements in their field, regardless of geographical location.
Continuing education is essential for professionals in the rapidly evolving field of neurointervention. Many organizations, including SNIS, offer continuing education courses, workshops, and certifications [30]. Through regular training and educational programs, neurointerventionalists from all specialties can hone their skills, acquire new techniques, and stay informed about recent research findings and technological advancements.
Another opportunity for knowledge exchange is through common grand rounds, where professionals from different specialties present clinical cases and share their perspectives, fostering cross-disciplinary learning. Multidisciplinary team meetings are another essential avenue for collaboration, as they allow specialists to discuss individual cases and develop comprehensive treatment plans. These meetings facilitate the identification of best practices, encourage consensus-building, and promote coordinated care. Additionally, joint clinical rotations can enhance understanding of the roles and contributions of other specialties in neurointervention, building a strong foundation for interdisciplinary practice.
Engaging professionals from various specialties in collaborative research projects can lead to innovative solutions and advancements in the field of neurointervention. Working together on research initiatives allows specialists to share their expertise and insights, fostering a culture of cooperation and mutual learning. Furthermore, developing interdisciplinary training programs can help bridge the gap between different specialties by providing education on the diverse aspects of neurointervention. These programs should focus on the unique contributions and skillsets of each specialty while emphasizing the importance of collaboration for optimal patient care. By bringing together specialists from various backgrounds, shared clinical facilities can optimize resource utilization, promote the exchange of ideas, and create a more efficient and effective healthcare environment. The integration of specialties in a shared setting may lead to better decision-making, improved patient care, and enhanced outcomes in the field of neurointervention.
Co-managed care
The co-managed care model has gained traction in various healthcare settings worldwide, demonstrating significant benefits for neurosurgical patients, including improved prognosis and recovery from ischemic stroke [32], subarachnoid hemorrhage [33], and head trauma [34]. The diverse perspectives and expertise of healthcare professionals, including neurointerventionalists, neuro-endovascular surgeons, neurointensivists, and other healthcare professionals, have resulted in better resource utilization and the establishment of effective emergency protocols [32].
Auerbach, et al. conducted a retrospective study that highlighted the positive impact of a co-managed care model involving neurosurgeons and hospitalists on neurosurgical patients, resulting in improved care quality, patient satisfaction, and reduced hospital costs [35]. Although the study showed minimal improvement in patient mortality and outcome, it underscores the potential benefits of co-managed care in advancing patient care. Josephson, et al. demonstrated the effectiveness of co-managed care in addressing specific variables such as fever, antibiotic use, and the diagnosis of ventilator-associated pneumonia, which were better managed through this collaborative approach [33]. Co-managed care has also been shown to enhance documentation and healthcare flow in neurosurgical intensive care units [34].
Various co-managed care models have been proposed and implemented to address the rising healthcare costs and potential decline in patient safety [36]. These models emphasize collaboration among healthcare professionals, such as neurointerventionalists, surgeons, and anesthesiologists, to provide comprehensive care for patients [36]. Interdisciplinary approaches, on the other hand, involve physicians from similar backgrounds working together to manage patient care [36]. Executive management teams typically oversee the recruitment of diverse medical and surgical representatives who bring unique value to clinical cases [37]. Improvements in care are often measured using quality metrics tailored to individual hospitals, including enhanced physician-to-physician communication and patient handoffs. Many hospitals have shifted from a centralized administration to allowing physicians greater autonomy in their workflow [37]. Current research advocates for flexibility within co-managed care models, encouraging hospitals to adapt these models to best meet the needs of their patients.
Furthermore, Comprehensive neurovascular centers provide optimal environments for patient treatment, as they offer access to various subspecialty care services. In addition to NIR, these centers ideally include neuroanesthesia, neuro-ICU care, and neurorehabilitation facilities, ensuring comprehensive care for patients with complex needs or complications following a procedure [38].
Occupational exposure
Occupational hazards such as exposure to ionizing radiation and wearing lead during procedures pose significant health risks to neurointerventional radiologists, including an increased risk of cancer and back pain [39]. These risks may limit the number of women in the field due to fear of radiation exposure, particularly during pregnancy [40]. To recruit more talented physicians and further expand the horizons of neurointervention, it is essential to explore solutions that minimize radiation exposure and overcome ergonomic obstacles.
Future of NIR
The development and implementation of robotic-assisted techniques offer significant potential for improving patient care, minimizing radiation exposure, and improving ergonomics in neurointervention. These innovations have shown promise in treating patients with severe symptomatic carotid stenosis and aneurysms of the basilar artery. In a recent Canadian study, a patient with a basilar trunk aneurysm underwent a stent-assisted coiling procedure with nearly all steps robotically performed, except for the manual placement of the guide-sheath and coaxial catheter [41]. The robot’s ease of use and smooth, precise movements facilitated navigation, stent placement, and coiling, demonstrating the potential for even greater robotic involvement in the future.
Using robotic-assisted techniques can reduce radiation exposure and ergonomic challenges faced by neurointerventional radiologists, leading to a more diverse and inclusive field that attracts a broader range of talented physicians. Furthermore, advancements in technology, such as sophisticated simulators and artificial intelligence (AI), will likely continue to enhance patient outcomes and reduce training differences among interventional practitioners. AI algorithms may help radiologists detect life-threatening neurological conditions more rapidly, such as ruptured aneurysms, aneurysm growth, and ischemic strokes [42-45]. Faster detection may lead to quicker neurovascular team notifications and improved patient outcomes.
As clinical trials continue to investigate the efficacy of robotic-assisted endovascular procedures, the adoption of this modality among practitioners has the potential to increase care coverage across the nation. Remote care delivery through robotic systems can provide access to specialty care in underserved areas [46-48]. However, healthcare facilities must address potential challenges, such as converting a robotic case to a manual case in case of complications or connectivity issues, before investing in this technology.
The implementation of robotic devices will require updates to the medical-legal framework and consideration of federal logistics and regulations regarding licenses, hours of coverage, and liability. As remote care becomes more widespread, it is essential to ensure that specialists are available to take over patient care in case of complications.
In summary, embracing robotic-assisted techniques and technology in neurointervention holds promise for improving patient care, attracting a more diverse pool of trainees, and expanding care coverage to underserved areas. By overcoming the challenges associated with implementing these advancements, the field of neurointervention can continue to grow and innovate.
- Chen M, Nguyen T. Emerging subspecialties in neurology: endovascular surgical neuroradiology. Neurology. 2008 Feb 5;70(6):e21-4. doi: 10.1212/01.wnl.0000299086.22147.89. PMID: 18250282.
- Gravino G. The pioneering past and cutting-edge future of interventional neuroradiology. Interv Neuroradiol. 2022 Oct 9:15910199221130234. doi: 10.1177/15910199221130234. Epub ahead of print. PMID: 36214159.
- Debrun G, Lacour P, Caron JP, Hurth M, Comoy J, Keravel Y. Inflatable and released balloon technique experimentation in dog -- application in man. Neuroradiology. 1975 Sep 15;9(5):267-71. doi: 10.1007/BF00333741. PMID: 1165852.
- Maingard J, Kok HK, Ranatunga D, Brooks DM, Chandra RV, Lee MJ, Asadi H. The future of interventional and neurointerventional radiology: learning lessons from the past. Br J Radiol. 2017 Dec;90(1080):20170473. doi: 10.1259/bjr.20170473. Epub 2017 Oct 3. PMID: 28972807; PMCID: PMC6047642.
- Guglielmi G. History of endovascular endosaccular occlusion of brain aneurysms: 1965-1990. Interv Neuroradiol. 2007 Sep;13(3):217-24. doi: 10.1177/159101990701300301. Epub 2007 Sep 15. PMID: 20566113; PMCID: PMC3345485.
- Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, Sandercock P; International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005 Sep 3-9;366(9488):809-17. doi: 10.1016/S0140-6736(05)67214-5. PMID: 16139655.
- Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, Pessin M, Ahuja A, Callahan F, Clark WM, Silver F, Rivera F. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999 Dec 1;282(21):2003-11. doi: 10.1001/jama.282.21.2003. PMID: 10591382.
- Fransen PS, Beumer D, Berkhemer OA, van den Berg LA, Lingsma H, van der Lugt A, van Zwam WH, van Oostenbrugge RJ, Roos YB, Majoie CB, Dippel DW; MR CLEAN Investigators. MR CLEAN, a multicenter randomized clinical trial of endovascular treatment for acute ischemic stroke in the Netherlands: study protocol for a randomized controlled trial. Trials. 2014 Sep 1;15:343. doi: 10.1186/1745-6215-15-343. PMID: 25179366; PMCID: PMC4162915.
- Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R; SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015 Jun 11;372(24):2285-95. doi: 10.1056/NEJMoa1415061. Epub 2015 Apr 17. PMID: 25882376.
- Gounis MJ, DeLeo MJ 3rd, Wakhloo AK. Advances in interventional neuroradiology. Stroke. 2010 Feb;41(2):e81-7. doi: 10.1161/STROKEAHA.109.574319. Epub 2010 Jan 14. PMID: 20075339.
- Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW; MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015 Jan 1;372(1):11-20. doi: 10.1056/NEJMoa1411587. Epub 2014 Dec 17. Erratum in: N Engl J Med. 2015 Jan 22;372(4):394. PMID: 25517348.
- Alberts MJ, Range J, Spencer W, Cantwell V, Hampel MJ. Availability of endovascular therapies for cerebrovascular disease at primary stroke centers. Interv Neuroradiol. 2017 Feb;23(1):64-68. doi: 10.1177/1591019916678199. Epub 2016 Nov 30. PMID: 27895242; PMCID: PMC5305162.
- Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, Sila CA, Hassan AE, Millan M, Levy EI, Mitchell P, Chen M, English JD, Shah QA, Silver FL, Pereira VM, Mehta BP, Baxter BW, Abraham MG, Cardona P, Veznedaroglu E, Hellinger FR, Feng L, Kirmani JF, Lopes DK, Jankowitz BT, Frankel MR, Costalat V, Vora NA, Yoo AJ, Malik AM, Furlan AJ, Rubiera M, Aghaebrahim A, Olivot JM, Tekle WG, Shields R, Graves T, Lewis RJ, Smith WS, Liebeskind DS, Saver JL, Jovin TG; DAWN Trial Investigators. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N Engl J Med. 2018 Jan 4;378(1):11-21. doi: 10.1056/NEJMoa1706442. Epub 2017 Nov 11. PMID: 29129157.
- Jabbour P, Tjoumakaris S, Chalouhi N, Randazzo C, Gonzalez LF, Dumont A, Rosenwasser R. Endovascular treatment of cerebral dural and pial arteriovenous fistulas. Neuroimaging Clin N Am. 2013 Nov;23(4):625-36. doi: 10.1016/j.nic.2013.03.010. Epub 2013 May 16. PMID: 24156854.
- Hwang H, La YK, Baek MS, Baik K, Suh SH, Kim WJ. Dural Arteriovenous Fistula Manifested as Rapid Progressive Dementia Successfully Treated by Endovascular Embolization Only. Neurointervention. 2017 Mar;12(1):50-53. doi: 10.5469/neuroint.2017.12.1.50. Epub 2017 Mar 6. PMID: 28316870; PMCID: PMC5355462.
- Iampreechakul P, Lertbutsayanukul P, Wattanasen Y, Thiraworawong T, Komonchan S, Siriwimonmas S. Reversible Thalamic Dementia Caused by Venous Hypertension of Bilateral Thalami Resulting from Multiple Intracranial Dural Arteriovenous Fistulas Successfully Obliterated by Endovascular Treatment using Liquid Embolic Materials: A Case Report and Literature Review. Asian J Neurosurg. 2020 Feb 25;15(1):144-154. doi: 10.4103/ajns.AJNS_317_19. PMID: 32181190; PMCID: PMC7057878.
- Waldeck S, Chapot R, von Falck C, Froelich MF, Brockmann M, Overhoff D. A Comparative Evaluation of Standard and Balloon-Assisted Coiling of Intracranial Aneurysms Based on Neurophysiological Monitoring. J Clin Med. 2022 Jan 28;11(3):677. doi: 10.3390/jcm11030677. PMID: 35160124; PMCID: PMC8836763.
- Link TW, Rapoport BI, Paine SM, Kamel H, Knopman J. Middle meningeal artery embolization for chronic subdural hematoma: Endovascular technique and radiographic findings. Interv Neuroradiol. 2018 Aug;24(4):455-462. doi: 10.1177/1591019918769336. Epub 2018 May 2. PMID: 29720020; PMCID: PMC6050895.
- Rahman WT, Griauzde J, Chaudhary N, Pandey AS, Gemmete JJ, Chong ST. Neurovascular emergencies: imaging diagnosis and neurointerventional treatment. Emerg Radiol. 2017 Apr;24(2):183-193. doi: 10.1007/s10140-016-1450-x. Epub 2016 Oct 7. PMID: 27718098.
- Lavine SD, Cockroft K, Hoh B, Bambakidis N, Khalessi AA, Woo H, Riina H, Siddiqui A, Hirsch JA, Chong W, Rice H, Wenderoth J, Mitchell P, Coulthard A, Signh TJ, Phatorous C, Khangure M, Klurfan P, terBrugge K, Iancu D, Gunnarsson T, Jansen O, Muto M, Szikora I, Pierot L, Brouwer P, Gralla J, Renowden S, Andersson T, Fiehler J, Turjman F, White P, Januel AC, Spelle L, Kulcsar Z, Chapot R, Spelle L, Biondi A, Dima S, Taschner C, Szajner M, Krajina A, Sakai N, Matsumaru Y, Yoshimura S, Ezura M, Fujinaka T, Iihara K, Ishii A, Higashi T, Hirohata M, Hyodo A, Ito Y, Kawanishi M, Kiyosue H, Kobayashi E, Kobayashi S, Kuwayama N, Matsumoto Y, Miyachi S, Murayama Y, Nagata I, Nakahara I, Nemoto S, Niimi Y, Oishi H, Satomi J, Satow T, Sugiu K, Tanaka M, Terada T, Yamagami H, Diaz O, Lylyk P, Jayaraman MV, Patsalides A, Gandhi CD, Lee SK, Abruzzo T, Albani B, Ansari SA, Arthur AS, Baxter BW, Bulsara KR, Chen M, Delgado Almandoz JE, Fraser JF, Heck DV, Hetts SW, Hussain MS, Klucznik RP, Leslie-Mawzi TM, Mack WJ, McTaggart RA, Meyers PM, Mocco J, Prestigiacomo CJ, Pride GL, Rasmussen PA, Starke RM, Sunenshine PJ, Tarr RW, Frei DF, Ribo M, Nogueira RG, Zaidat OO, Jovin T, Linfante I, Yavagal D, Liebeskind D, Novakovic R, Pongpech S, Rodesch G, Soderman M, terBrugge K, Taylor A, Krings T, Orbach D, Biondi A, Picard L, Suh DC, Tanaka M, Zhang HQ. Training Guidelines for Endovascular Ischemic Stroke Intervention: An International Multi-Society Consensus Document. AJNR Am J Neuroradiol. 2016 Apr;37(4):E31-4. doi: 10.3174/ajnr.A4766. Epub 2016 Feb 18. PMID: 26892982; PMCID: PMC7960155.
- SNIS. How to Become a Neurointerventionalist [Available from: https://www.snisonline.org/pathways/
- Day AL, Siddiqui AH, Meyers PM, Jovin TG, Derdeyn CP, Hoh BL, Riina H, Linfante I, Zaidat O, Turk A, Howington JU, Mocco J, Ringer AJ, Veznedaroglu E, Khalessi AA, Levy EI, Woo H, Harbaugh R, Giannotta S. Training Standards in Neuroendovascular Surgery: Program Accreditation and Practitioner Certification. Stroke. 2017 Aug;48(8):2318-2325. doi: 10.1161/STROKEAHA.117.016560. Epub 2017 Jul 13. PMID: 28706116.
- Sauvageau E, Hopkins LN. Training in cerebrovascular disease: do we need to change the way we train residents? Neurosurgery. 2006 Nov;59(5 Suppl 3):S282-6; discussion S3-13. doi: 10.1227/01.NEU.0000237333.81543.D2. PMID: 17053614.
- de Vries J, Boogaarts HD. Treatment of patients with ruptured aneurysm by neurosurgeons that perform both open surgical and endovascular techniques is safe and effective: results of a single centre in Europe. Acta Neurochir (Wien). 2014 Jul;156(7):1259-66; discussion 1266. doi: 10.1007/s00701-014-2101-1. Epub 2014 May 1. PMID: 24789710.
- Gupta A, Reddy V, Barpujari A, Lavadi RS, Agarwal P, Chang YF, Mooney J, Elsayed GA, Agarwal N. Current Trends in Subspecialty Fellowship Training for 1691 Academic Neurological Surgeons. World Neurosurg. 2023 Mar;171:e47-e56. doi: 10.1016/j.wneu.2022.11.074. Epub 2022 Nov 18. PMID: 36403934.
- Chewning R, Wyse G, Murphy K. Neurointervention for the peripheral radiologist: tips and tricks. Semin Intervent Radiol. 2008 Mar;25(1):42-7. doi: 10.1055/s-2008-1052305. PMID: 21326492; PMCID: PMC3036406.
- Liang CW, Das S, Ortega-Gutierrez S, Liebeskind DS, Grotta JC, Jovin TG, Nguyen TN, Nogueira RG, Masoud H, Elijovich L, Zaidat OO, Hassan AE, Linfante I, Fifi JT, Sheth SA. Education Research: Challenges Faced by Neurology Trainees in a Neuro-Intervention Career Track. Neurology. 2021 Apr 13;96(15):e2028-e2032. doi: 10.1212/WNL.0000000000011629. Epub 2021 Feb 12. PMID: 33579757.
- Cox M, Atsina KB, Sedora-Roman NI, Pukenas BA, Parker L, Levin DC, Bagley LJ, Hurst RW. Neurointerventional Radiology for the Aspiring Radiology Resident: Current State of the Field and Future Directions. AJR Am J Roentgenol. 2019 Apr;212(4):899-904. doi: 10.2214/AJR.18.20336. Epub 2019 Jan 30. PMID: 30699013.
- Itsekzon-Hayosh Z, Agid R. Diversity among endovascular neurointerventionalists in Canada results of a national survey 2022. Interv Neuroradiol. 2023 Mar 27:15910199231164838. doi: 10.1177/15910199231164838. Epub ahead of print. PMID: 36972494.
- SNIS. [Available from: https://www.snisonline.org/.
- Elkind MSV, O'Gara P. Clinical Practice Guidelines in Interventional Neurology: Mind the GAPS. Stroke: Vascular and Interventional Neurology. 2021; 1(1):e000225.
- Bershad EM, Feen ES, Hernandez OH, Suri MF, Suarez JI. Impact of a specialized neurointensive care team on outcomes of critically ill acute ischemic stroke patients. Neurocrit Care. 2008;9(3):287-92. doi: 10.1007/s12028-008-9051-5. PMID: 18196476.
- Josephson SA, Douglas VC, Lawton MT, English JD, Smith WS, Ko NU. Improvement in intensive care unit outcomes in patients with subarachnoid hemorrhage after initiation of neurointensivist co-management. J Neurosurg. 2010 Mar;112(3):626-30. doi: 10.3171/2009.8.JNS09441. PMID: 19731990.
- Varelas PN, Eastwood D, Yun HJ, Spanaki MV, Hacein Bey L, Kessaris C, Gennarelli TA. Impact of a neurointensivist on outcomes in patients with head trauma treated in a neurosciences intensive care unit. J Neurosurg. 2006 May;104(5):713-9. doi: 10.3171/jns.2006.104.5.713. PMID: 16703875.
- Auerbach AD, Wachter RM, Cheng HQ, Maselli J, McDermott M, Vittinghoff E, Berger MS. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010 Dec 13;170(22):2004-10. doi: 10.1001/archinternmed.2010.432. PMID: 21149758.
- Retchin SM. A conceptual framework for interprofessional and co-managed care. Acad Med. 2008 Oct;83(10):929-33. doi: 10.1097/ACM.0b013e3181850b4b. PMID: 18820522.
- Yan J, Gilbert JH, Hoffman SJ. World Health Organization Study Group on Interprofessional Education and Collaborative Practice. J Interprof Care. 2007 Dec;21(6):588-9. doi: 10.1080/13561820701775830. PMID: 18038291.
- Hui FK, Spiotta AM, Katzan I, Manno EM, Masaryk TJ, Rasmussen PA. Evolution of a multidisciplinary cerebrovascular center: lessons learned. J Neurointerv Surg. 2012 Mar;4(2):147-51. doi: 10.1136/jnis.2010.004101. Epub 2011 May 11. PMID: 21990440.
- Weisz G, Metzger DC, Caputo RP, Delgado JA, Marshall JJ, Vetrovec GW, Reisman M, Waksman R, Granada JF, Novack V, Moses JW, Carrozza JP. Safety and feasibility of robotic percutaneous coronary intervention: PRECISE (Percutaneous Robotically-Enhanced Coronary Intervention) Study. J Am Coll Cardiol. 2013 Apr 16;61(15):1596-600. doi: 10.1016/j.jacc.2012.12.045. PMID: 23500318.
- Vu CT, Elder DH. Pregnancy and the working interventional radiologist. Semin Intervent Radiol. 2013 Dec;30(4):403-7. doi: 10.1055/s-0033-1359735. PMID: 24436568; PMCID: PMC3835582.
- Mendes Pereira V, Cancelliere NM, Nicholson P, Radovanovic I, Drake KE, Sungur JM, Krings T, Turk A. First-in-human, robotic-assisted neuroendovascular intervention. J Neurointerv Surg. 2020 Apr;12(4):338-340. doi: 10.1136/neurintsurg-2019-015671.rep. Epub 2020 Mar 3. PMID: 32132138; PMCID: PMC7146920.
- Morey JR, Zhang X, Yaeger KA, Fiano E, Marayati NF, Kellner CP, De Leacy RA, Doshi A, Tuhrim S, Fifi JT. Real-World Experience with Artificial Intelligence-Based Triage in Transferred Large Vessel Occlusion Stroke Patients. Cerebrovasc Dis. 2021;50(4):450-455. doi: 10.1159/000515320. Epub 2021 Apr 13. PMID: 33849032.
- Yahav-Dovrat A, Saban M, Merhav G, Lankri I, Abergel E, Eran A, Tanne D, Nogueira RG, Sivan-Hoffmann R. Evaluation of Artificial Intelligence-Powered Identification of Large-Vessel Occlusions in a Comprehensive Stroke Center. AJNR Am J Neuroradiol. 2021 Jan;42(2):247-254. doi: 10.3174/ajnr.A6923. Epub 2020 Dec 31. PMID: 33384294; PMCID: PMC7872164.
- Silva MA, Patel J, Kavouridis V, Gallerani T, Beers A, Chang K, Hoebel KV, Brown J, See AP, Gormley WB, Aziz-Sultan MA, Kalpathy-Cramer J, Arnaout O, Patel NJ. Machine Learning Models can Detect Aneurysm Rupture and Identify Clinical Features Associated with Rupture. World Neurosurg. 2019 Nov;131:e46-e51. doi: 10.1016/j.wneu.2019.06.231. Epub 2019 Jul 9. PMID: 31295616.
- Shimada Y, Tanimoto T, Nishimori M, Choppin A, Meir A, Ozaki A, Higuchi A, Kosaka M, Shimahara Y, Kitamura N. Incidental cerebral aneurysms detected by a computer-assisted detection system based on artificial intelligence: A case series. Medicine (Baltimore). 2020 Oct 23;99(43):e21518. doi: 10.1097/MD.0000000000021518. PMID: 33120725; PMCID: PMC7581039.
- Panesar SS, Volpi JJ, Lumsden A, Desai V, Kleiman NS, Sample TL, Elkins E, Britz GW. Telerobotic stroke intervention: a novel solution to the care dissemination dilemma. J Neurosurg. 2019 Nov 29;132(3):971-978. doi: 10.3171/2019.8.JNS191739. PMID: 31783366.
- Legeza P, Britz GW, Loh T, Lumsden A. Current utilization and future directions of robotic-assisted endovascular surgery. Expert Rev Med Devices. 2020 Sep;17(9):919-927. doi: 10.1080/17434440.2020.1814742. Epub 2020 Aug 31. PMID: 32835546.
- Rabinovich EP, Capek S, Kumar JS, Park MS. Tele-robotics and artificial-intelligence in stroke care. J Clin Neurosci. 2020 Sep;79:129-132. doi: 10.1016/j.jocn.2020.04.125. Epub 2020 Aug 5. PMID: 33070881.