More Information
Submitted: September 08, 2023 | Approved: September 14, 2023 | Published: September 15, 2023
How to cite this article: Issa CJ, Nasser B, Mazraani B, Eid KT, Loving B, et al. Acute Inflammatory Reaction After Radiotherapy to Bilateral Orbital Metastasis from Melanoma. J Radiol Oncol. 2023; 7: 056-057.
DOI: 10.29328/journal.jro.1001054
Copyright License: © 2023 Issa CJ, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Acute Inflammatory Reaction After Radiotherapy to Bilateral Orbital Metastasis from Melanoma
Christopher J Issa1, Batoul Nasser2*, Batoul Mazraani1, Kevin T Eid1, Bailey Loving3, Thomas J Quinn3 and Muayad F Almahariq4
1Oakland University William Beaumont School of Medicine, USA 2Trinity Health Hospital, Livonia, USA 3Corewell Health, USA 4Beaumont Health, USA
*Address for Correspondence: Batoul Nasser, MD, Trinity Health Hospital Livonia, USA, Email: [email protected]
Orbital melanoma is a subtype of periocular melanoma that can present from primary, secondary (arising from local invasion), or metastatic disease [1]. Melanoma metastasis to the orbit is rare with the majority of metastases occurring in subcutaneous tissue, nonregional lymph nodes, lungs, liver, brain, and bone [2]. Despite melanoma being relatively radioresistant, radiation therapy can be considered in an adjuvant or palliative setting [3]. In the palliative setting specifically, radiation therapy is highly effective in alleviating symptoms due to mass effect [3]. However, significant ocular and orbital complications may occur as a direct result of radiation therapy.
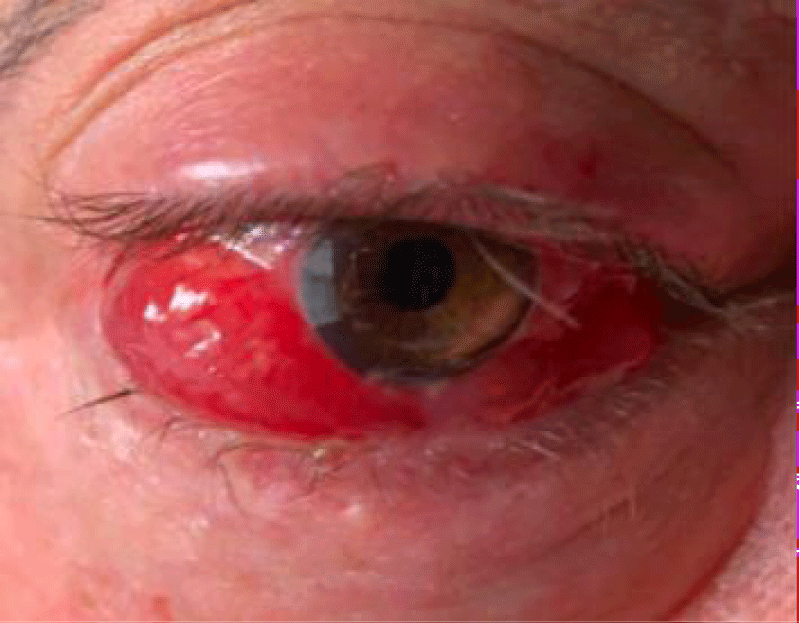
A man in his 50s with stage IV primary cutaneous melanoma with bilateral orbital metastases developed tumor progression despite two orbitotomies for oncologic resection, one-year treatment with ipilimumab and nivolumab, and three cycles of temozolomide. A plan was made to treat the right orbital mass with palliative radiation therapy to a dose of 30 gray (Gy) in 10 fractions. Four hours following his first fraction of radiation therapy, he developed severe right eye pain unresponsive to non-steroidal anti-inflammatory drugs. Eye examination was notable for injection, chemosis, proptosis, hyperglobus of the right eye with mucoid discharge, and right ophthalmoplegia with incomplete eyelid closure (Figure 1). Ophthalmological examination demonstrated preservation of color vision, brightness perception, and visual acuity.
Figure 1: Redness, chemosis, proptosis, and hyperglobus of the right eye with mucoid discharge four hours after the patient’s first radiation therapy.
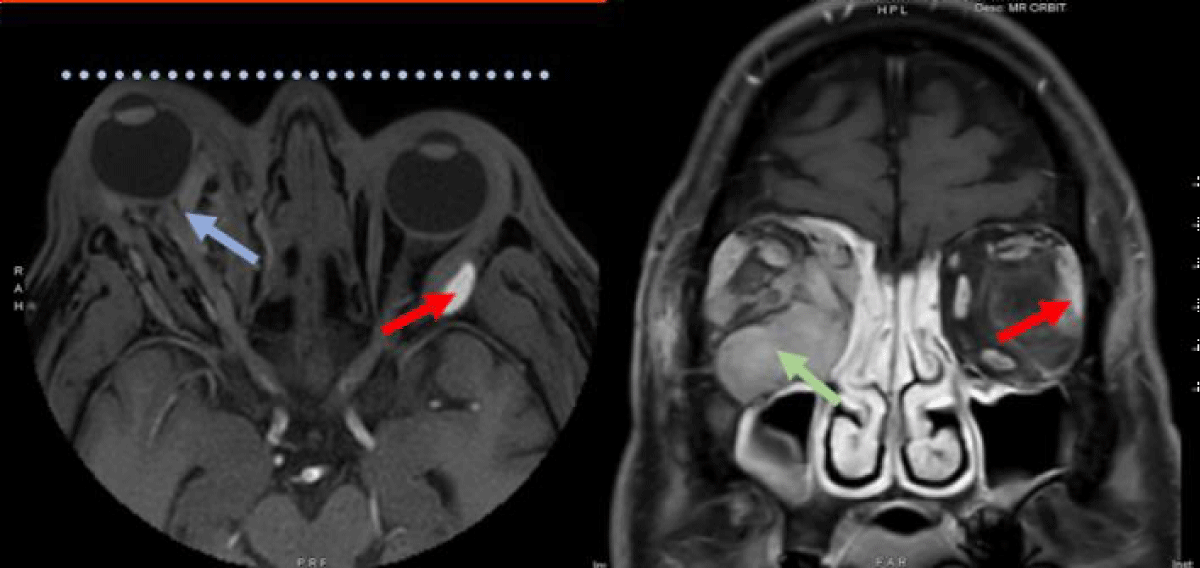
MRI of the orbits demonstrated progression of his right orbital mass with increased proptosis, a stretched appearance of the optic nerve, and tethering of the posterior globe with a stable left orbital mass (Figure 2). This acute swelling of the right orbital mass was deemed to be likely related to an inflammatory reaction to his first radiation treatment. Intravenous dexamethasone at a dose of four milligrams was administered with significant improvement in ocular symptoms. He was discharged with a 9-day oral dexamethasone taper along with dorzolamide/timolol eye drops, brimonidine eye drops and Lacri-Lube ointment.
Figure 2: Axial (left) and coronal (right) T1 MRI images with contrast demonstrating greater right eye proptosis (dotted line) with a stretched appearance of the optic nerve and tethering of the posterior globe (blue arrow). Increased swelling due to acute inflammatory reaction in the right orbital mass (green arrow). The left orbital mass remains stable (red arrow).
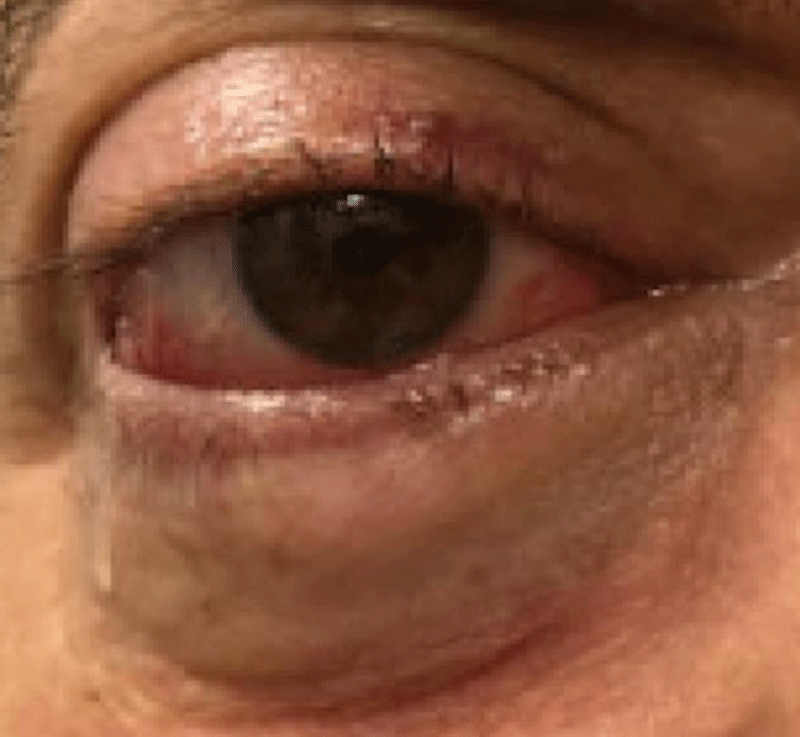
The patient proceeded with radiation therapy as planned and tolerated the remainder of his treatments with gradual improvement in his right eye pain and swelling. One month following radiation therapy, the patient’s proptosis, hyperglobus, and chemosis were mildly improved and temozolomide was restarted (Figure 3). MRI of the orbits two months following radiation therapy showed an interval decrease in the size of the bilateral orbital masses and continued improvement in right eye proptosis (Figure 4).
Figure 3: Improvement in redness, proptosis, hyperglobus, and chemosis of the patient’s right eye two months following radiation therapy.
Figure 4: Axial (left) and sagittal (right) T1 MRI images with contrast demonstrating a mild decrease in the size of the large right-sided intra-orbital mass (blue arrow) with improvement of proptosis two months following radiation therapy.
Orbital metastases from any malignancy are relatively rare, with metastatic melanoma accounting for approximately 5-20% of all cases [2]. Treatment often involves immunotherapy, chemotherapy, and radiation therapy, however, the prognosis remains poor [4]. Radiation therapy is especially beneficial for patients who are unable to undergo surgery, yet require tumor control for preservation of vision and palliation of pain [5]. Orbital radiotherapy has been shown to reduce tumor load and alleviate orbital symptoms with long-term toxicity including cataracts, optic neuropathy, radiation retinopathy, and corneal scarring [4]. However, radiation can also induce an acute inflammatory response leading to swelling and an increase in tumor size following treatment [6]. Though this sterile inflammatory response can lead to unwanted symptoms, the increase in inflammatory cells following radiation is important in killing tumor cells. Therefore, the symptoms of inflammation did not rule out further treatment for this patient but were a sign that the therapeutic effects of radiation were occurring; however, the effects of edema need to be controlled to limit the compressive effects of important vessels such as the optic nerve.
Radiation therapy activates pro- and anti-inflammatory signaling pathways, stimulating the immune system and leading to tumor cell death [6]. While one of the goals of radiation therapy is aimed at modulating anti-tumor immune responses, it may also stimulate factors that contribute to excess inflammation, fibrosis, and tumor invasion [6]. Ionizing radiation activates several immunological proteins and transcription factors, such as nuclear factor kappa B (NF-kB), tumor necrosis factor-alpha (TNF-a), interleukin-1 (IL-1), IL-6 and IL-8 [6]. These transcription factors and cytokines play a major role in the regulation of genes that stimulate inflammatory and angiogenic processes [6]. Radiation therapy can also further indirectly induce inflammation through NF-kB activation of cyclooxygenase-2 (COX-2), which is one of the key enzymes in the inflammatory cascade [6].
In our case, the rapid increase in size and enhancement on an MRI points to an inflammatory reaction due to radiation therapy. The efficacy of corticosteroids further implicates inflammation as the pathological cause, supporting the role of anti-inflammatory agents for future treatments. It is imperative to identify radiation-induced inflammation in tumors to promptly initiate treatment to prevent optic nerve damage and provide adequate relief of symptoms.
- Rose AM, Luthert PJ, Jayasena CN, Verity DH, Rose GE. Primary Orbital Melanoma: Presentation, Treatment, and Long-term Outcomes for 13 Patients. Front Oncol. 2017 Dec 18;7:316. doi: 10.3389/fonc.2017.00316. PMID: 29326884; PMCID: PMC5741819.
- Rose AM, Cowen S, Jayasena CN, Verity DH, Rose GE. Presentation, Treatment, and Prognosis of Secondary Melanoma within the Orbit. Front Oncol. 2017 Jun 23;7:125. doi: 10.3389/fonc.2017.00125. PMID: 28690979; PMCID: PMC5481311.
- Shi W. Radiation Therapy for Melanoma. In: Ward WH, Farma JM, editors. Cutaneous Melanoma: Etiology and Therapy [Internet]. Brisbane (AU): Codon Publications; 2017 Dec 21. Chapter 8. PMID: 29461772.
- Greene DP, Shield DR, Shields CL, Shields JA, Servat JJ, Lin CJ, Douglass AM, Fulco EA, Levin F. Cutaneous melanoma metastatic to the orbit: review of 15 cases. Ophthalmic Plast Reconstr Surg. 2014 May-Jun;30(3):233-7. doi: 10.1097/IOP.0000000000000075. PMID: 24811686.
- Ioakeim-Ioannidou M, MacDonald SM. Evolution of Care of Orbital Tumors with Radiation Therapy. J Neurol Surg B Skull Base. 2020 Aug;81(4):480-496. doi: 10.1055/s-0040-1713894. Epub 2020 Aug 24. PMID: 33072488; PMCID: PMC7561458.
- Di Maggio FM, Minafra L, Forte GI, Cammarata FP, Lio D, Messa C, Gilardi MC, Bravatà V. Portrait of inflammatory response to ionizing radiation treatment. J Inflamm (Lond). 2015 Feb 18;12:14. doi: 10.1186/s12950-015-0058-3. PMID: 25705130; PMCID: PMC4336767.